A 20 YRS OLD MALE CAME TO OPD WITH CHIEF COMPLAINTS OF YELLOWISH DISCOLORATION OF EYES
E LOG GENERAL MEDICINE.
Hi, I am Anvitha,5th Sem Medical Student. This is an online e-log book to discuss our patient's health data shared after taking his/her/guardian's consent . This also reflects patient centered care and online learning portfolio.
- This E-log book also reflects my patient-centered online learning portfolio and of course, your valuable inputs and feedbacks are most welcome through the comments box provided at the very end. HAPPY READING.
- * This is an ongoing case. I am in the process of updating and editing this ELOG as and when required
CASE SHEET.
Chief complaints and duration.
A 20 yrs old male came to opd with chief complaints of Yellowsish discoloration of eyes.
History of present illness.
patient was apparently asymptimatic since one year back then developed Yellowsish discoloration of eyes
POSITIVE HISTORY
Loss of appetite
Irregular bowel and bladder movements
Adipsia
NEGATIVE HISTORY:
N/K/C/O: TB , Asthma, epilepsy, thyroid
Personal history.
Mixed diet
Irregular bowel and bladder movements
Adipsia
No addictions
Sleep adequate
Family history.
No significant family history.
PHYSICAL EXAMINATION.
A. General Examination
The patient was conscious coherent and well oriented to time place and person and was examined in a well lit room.
Pallor is absent.
Icterus is absent
No cyanosis
No clubbing of fingers
No lymphadenopathy
No malnutrition
No clubbing of fingers
No oedema of feet and hands.
VITALS:
Temperature :afebrile
Pulse:86bpm
Bp:100/70 mmhg
SYSTEMIC EXAMINATION
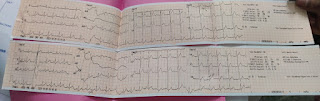
B. Cardiovascular system
No thrills
No cardiac murmurs
Cardiac sounds: S1 and S2
C. Respiratory system
dyspnea absent
No wheezing
Vesicular breath sounds
Position of trachea - central
D. Abdomen
Abdomen is scaphoid
No tenderness
No Palpable mass
Bowel sounds are present
No bruits
No free fluids
E. Central nervous system
The patient was conscious coherent and cooperative.
No neck stiffness
No kernick sign
Speech normal
Tone Rt Lt
UL N N
LL N N
Power Rt Lt
UL 5/5 5/5
LL 5/5 4/5
Provisional diagnosis:Patient was diagnosed with secondary jaundice.









Comments
Post a Comment