65 year old male patient presented with reduced urine output and generalised swelling.
E LOG GENERAL MEDICINE.
Hi, I am Anvitha, 3rd Sem Medical Student. This is an online e-log book to discuss our patient's health data shared after taking his/her/guardian's consent . This also reflects patient centered care and online learning portfolio.
- This E-log book also reflects my patient-centered online learning portfolio and of course, your valuable inputs and feedbacks are most welcome through the comments box provided at the very end. HAPPY READING.
- * This is an ongoing case. I am in the process of updating and editing this ELOG as and when required
CASE SHEET.
Chief complaints and duration.
A 65 year old male patient who was previously a farmer by profession came to the opd with the chief complains of reduced urine output and generalised swelling since ten days and shortness of breath since ten days.
History of present illness.
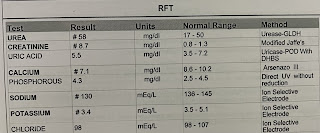
Patient was apparently asymptomatic four years back and then suddenly developed pain in abdomen and tightness and came to the hospital for which he came to the hospital and diagnosed with renal caliculi. He underwent percutaneous nephrostomy and later discharged. He later developed generalised weakness and dizziness for which he was diagnosed with high blood pressure two years back and was on irregular medication. And two years ago on being unresponsive, he was in ICU for 4-5 days and diagnosed to be hypoglycaemic and creatinine level was 5.94. On recommending dialysis he refused it and got discharged. He has pedal oedema on and off. He had loose stools 10 days back and decreased urine out put for one day and anuria for three days and underwent haemodialasis.
History of past illness.
Diabetic since 2 years.
Hypertension since 2 years.
Personal history.
Patient was previously a farmer by occupation.
Bowel movement is regular.
Anuria.
No history of Allergy.
Smoking since past 6 years stopped 10 days back.
Drinking
Family history.
No significant family history.
PHYSICAL EXAMINATION.
A. General Examination
Pallor is present.
Icterus is seen.
No cyanosis
No clubbing of fingers
No lymphadenopathy
No malnutrition
No clubbing of fingers
oedema of feet and hands.
Temperature:
Pulse:
Respiration:
SYSTEMIC EXAMINATION
B. Cardiovascular system
No thrills
No cardiac murmurs
Cardiac sounds: S1 and S2
C. Respiratory system
No dyspnea
No wheezing
Vesicular breath sounds .
D. Abdomen
Abdomen is Obese
No tenderness
No Palpable mass
The patient was conscious coherent and cooperative.










Comments
Post a Comment